The Dallas-based Parkland Center for Clinical Innovation has developed a new Vulnerability Index to analyze what ZIP codes in Dallas County are most at risk for COVID-19 infection.
County and city health officials are already using the tool to help prioritize resources that could slow potential growth in infections, PCCI said. In identifying COVID-19 hot spots and long-term risk factors, the PCCI Vulnerability Index can give decision-makers information to identify communities most in need.
The PCCI Vulnerability Index took a whole team, led by Dr. Tom Roderick (PCCI Sr. Data Scientist) and Yolande Pengetnze (PCCI Medical Director), and about 45 days to develop. Dr. Steve Miff, PCCI’s CEO and president, served as the vision behind the project as its executive sponsor—PCCI said he “likes to get his hands dirty occasionally and as often as time permits.”
PCCI also worked in close collaboration with the DFW Hospital Council and Dallas County Health and Human Services and received input from Dr. Baggett, the City of Dallas’ COVID Czar; Dr. Brett Moran, CMIO of Parkland; and a consortium of North Texas thought leaders.
Version 1 is now complete, but Dr. Miff said there’s a vision and aspiration to continue evolving the index. “The Vulnerability Index, since it’s more stable, will be updated monthly. The rising risk, hot-spotting of the most recent confirmed COVID-19 cases, will be updated weekly,” he told Dallas Innovates.
Targeted community interventions can impact a region’s experience with a COVID-19 outbreak, according to PCCI.
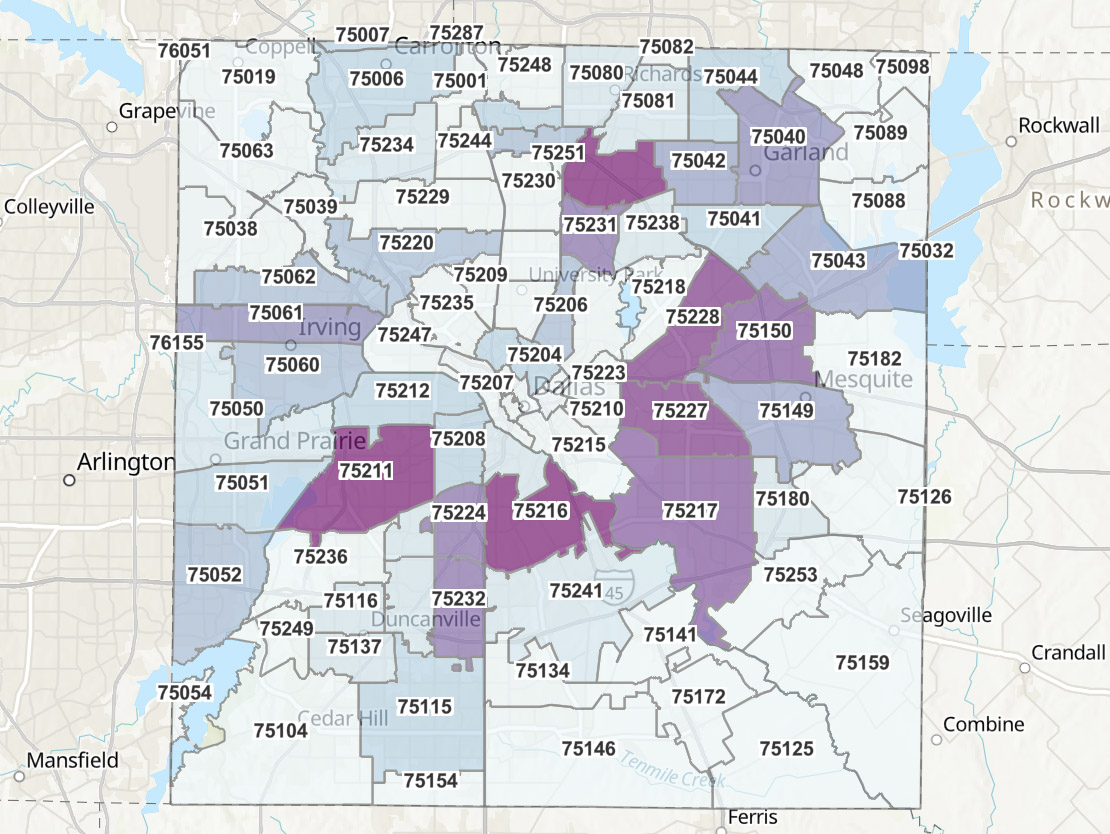
PCCI Vulnerability Index [Map: Courtesy PCCI]
The PCCI Vulnerability Index takes into account a variety of risk factors—social, clinical, and demographic—to capture both individual and synergistic risk factors.
Dr. Miff breaks it down.
“The tool is meant to help healthcare providers, local public health officials, and city and county leaders coordinate efforts to address the rapidly changing pandemic,” Dr. Miff says.
Its primary aims include where testing needs to be deployed, outreach for high-risk areas, and adjusted forecast models, according to Dr. Miff:
• “Identify and prioritize where testing needs to be deployed based not only on the vulnerability of an area, but the real-time rising risk driven by confirmed cases
• Develop targeted education and outreach for high-risk areas that are culturally sensitive based on the demographic and ethnic composition of those areas; inform the downstream impact of the virus
• Help capacity modeling teams adjust forecast models based on the dynamic evolution of the disease.”
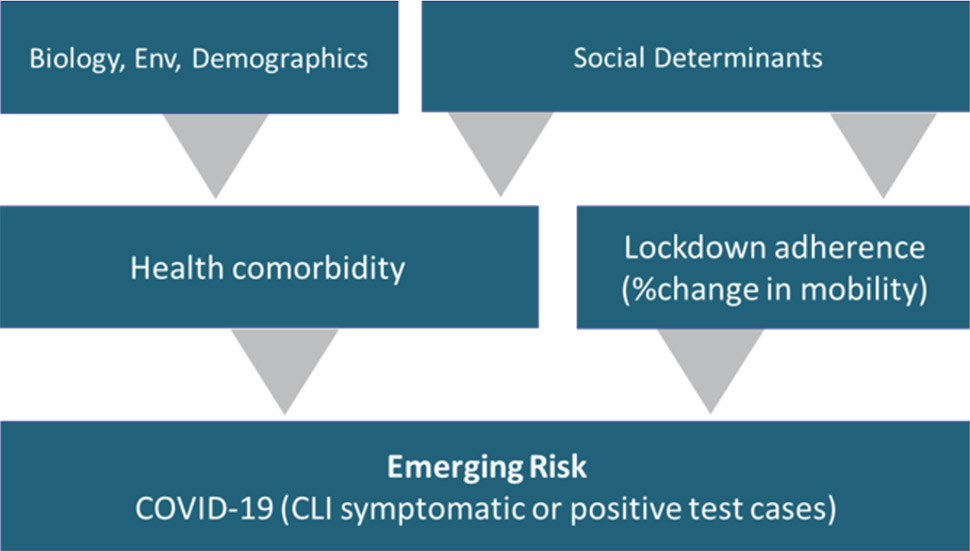
Risk factors per PCCI [Image: Courtesy PCCI]
The takeaway? “The PCCI Vulnerability Index is robust and highly correlated with COVID-19 incidence, more so than its individual components,” PCCI said. “The amount of patients in a ZIP code that have a known COVID-19 comorbidity is the strongest sub-component of the index.”
PCCI discovered major differences occurred between race and ethnic groups when it came to a community’s experience with COVID-19. Those differences appear to be strongly related to socioeconomic deprivations.
For example, mobility and socioeconomic deprivation are highly correlated, the analysis shows. Socioeconomic factors that could affect mobility include crowded living conditions and the type and industry of work. That could make both a potential target for community and public health interventions.
Dallas Innovates dives into the Vulnerability Index to see what factors PCCI uncovered that could contribute to Dallas’ COVID-19 risk. Read on for a deeper analysis.
PCCI’s Vulnerability Index: A closer look
PCCI focused on data science and clinical expertise to improve health for vulnerable populations. Using advanced analytics, geospatial modeling (hot-spotting), and integrated patient-management tools, PCCI hopes to mitigate the surge and save lives until treatments and vaccines are available.
“We developed the Vulnerability Index as a way to assist community and healthcare leaders to address the factors that cause COVID-19’s exponential spread,” PCCI said. “By analyzing the geospatial distribution of COVID-19 risk factors PCCI is able to identify communities especially at risk for COVID-19, allowing for targeted community support and intervention.”
In all, PCCI wanted to build an index that comprehensively captured the social, clinical, and public health complexity of COVID-19. The intent was to make it evidence-based, equitable, practical, and actionable so local communities and public health leaders could use it easily.
According to PCCI, its Vulnerability Index has strong validity when it comes to capturing a community’s COVID-19 risk.
It’s easy to discern: The higher the index, the higher the risk of COVID-19 infection.
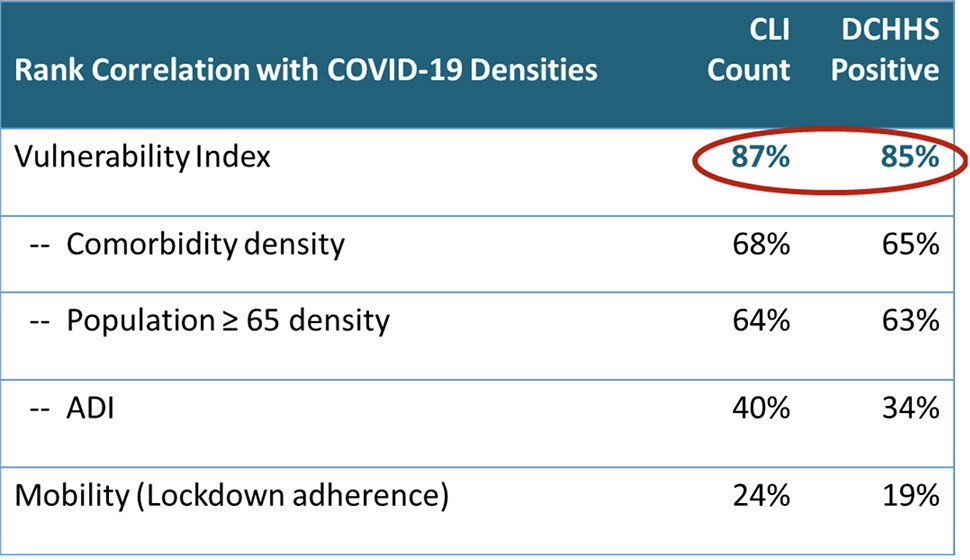
[Graph: Courtesy PCCI]
The risk factors that PCCI took into account are strongly correlated with COVID-19 infection, such as comorbidities, age, social deprivation, and mobility. But the “PCCI Vulnerability” has the strongest association with a community’s COVID-19 risk, because PCCI said its index captures each risk factor’s individual effect as well as synergies across risk factors.
“Racial and ethnic disparities exist in COVID-19 risk and are closely aligned with social deprivation, as measured by the ADI,” PCCI said. “Hispanic and African American neighborhoods are at the highest risk for COVID-19.”
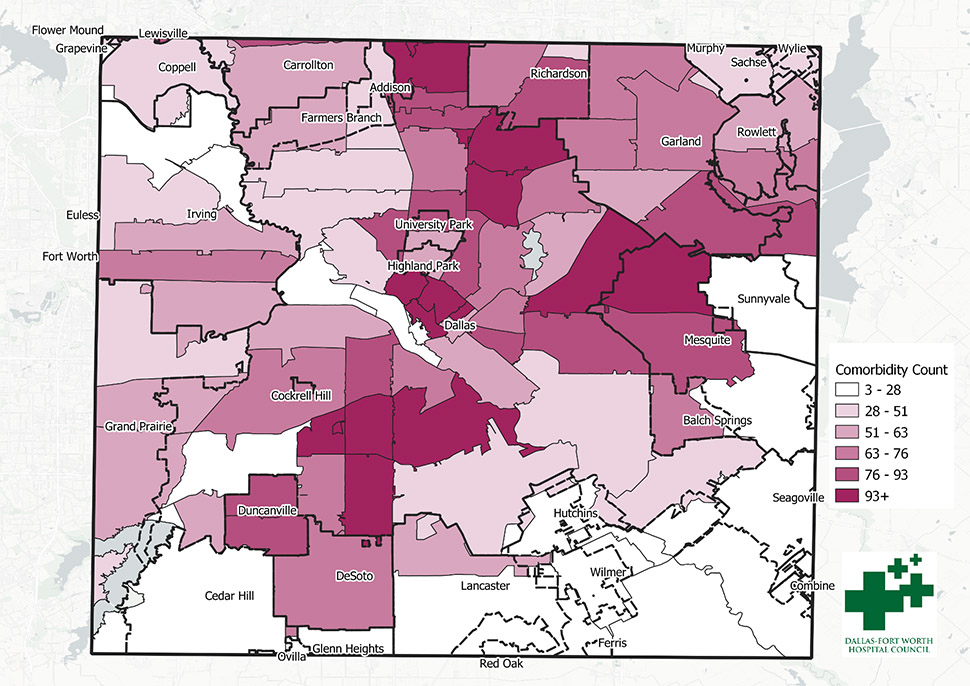
COVID-19 Comorbidity Patient Distribution [Map: Courtesy PCCI]
PCCI compares COVID-19 response to fire prevention: Emergency management has long-term considerations, like where to locate a firehouse, and short-term, like identifying active fires.
Some community factors—such as people with chronic diseases, poverty, a high number of elderly—can’t be addressed in the short-term.
PCCI incorporated these factors into the Vulnerability Index because they are known for higher COVID-19 risk. But, simply because a risk factor is connected to COVID-19 doesn’t mean that risk factor causes COVID-19.
For example, socioeconomic distress doesn’t cause COVID-19, but people facing hard economic times may not be able to adhere to public health recommendations, like working from home.
“This presents an intervention opportunity for public health and community leaders—by addressing a community’s ability to lock down, through increased testing and disease identification sites, rent or mortgage moratoriums, food distribution, utility forgiveness, and other basic needs assistance, community leaders can decouple a community’s COVID-19 risk from economic distress,” PCCI said.
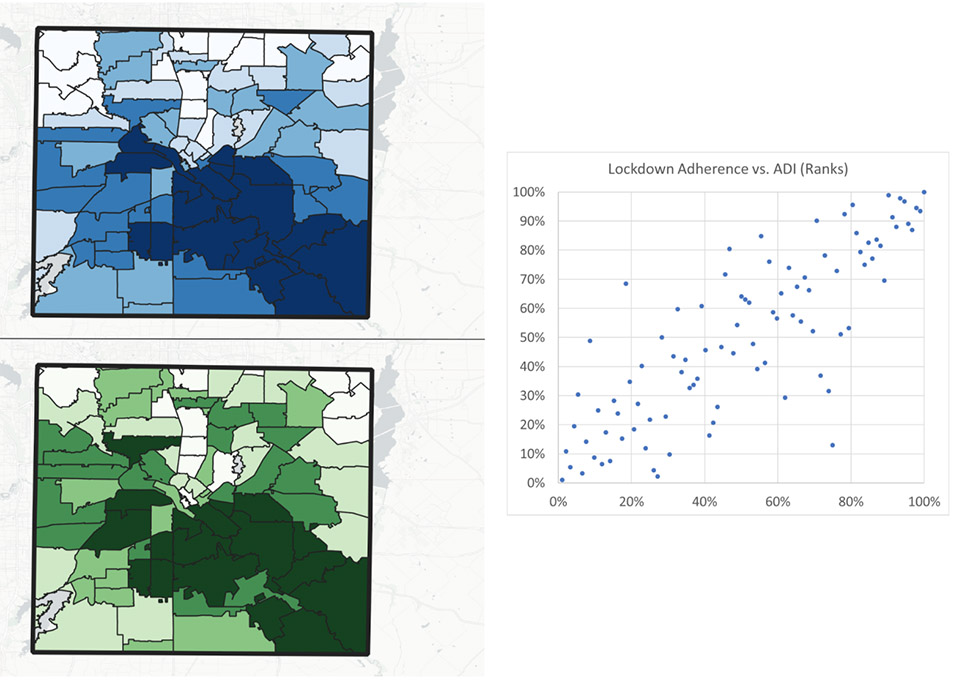
Social Distancing in Dallas County: Lockdown adherence (top) versus area deprivation (bottom). Population was weighted by Census Blockgroup. Scatterplot on the right. [Maps: Courtesy PCCI]
As for long-term factors, PCCI’s Vulnerability Index aims to “open the door” for communities to better understand their risk and figure out where to put resources.
Emerging risk is wherever current COVID-19 cases are and where those patients work, play, worship, and live. Incorporating COVID-19 hotspot information with anonymous, aggregated mobility data allows communities to identify the places needing urgent attention.
Then, PCCI said, public health actions can be taken: culturally appropriate media messaging via radio, television, and social media; community-based focus messaging; canvassing; contract-tracing starting points such as places of worship, barbershops, and grocery stores; and pop-up testing site location decision making.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.