Children’s Health in Dallas is one of the leading pediatric heart centers in the nation and recently, the health system showcased the people and the equipment that are saving lives during its first Innovation Expo.
The Heart Center at Children’s Health offers some of the leading pediatric cardiologists, surgeons, and researchers affiliated with UT Southwestern Medical Center, as well as cutting-edge equipment used to treat some of the most-difficult cardiac cases.
The center is all about saving lives.
One of the new programs with that mission, Safe at Home, is proving to be successful in helping children with complex congenital heart conditions and their families deal with the time between the multiple operations the child may need during their first years of life.
Those procedures often require lengthy hospital stays that disrupt the family’s life and strain the child and their family.
The Heart Center at Children’s Health recently made an important addition to the Safe at Home program — Building HOPE (Healthy Outcomes through Parent Engagement).
“Our goal is to drive it [mortality rate] as close to zero as we possibly can.”
Dr. Thomas Zellers
It’s a tablet-based platform that helps with the intensive home monitoring that patients need by improving communication of specific monitoring patterns from parent to the cardiology team at the Heart Center.
“Prior to the Safe at Home Program, the mortality rate in our institution of a child who had a Norwood operation, got out of the hospital, and went home was 17 percent chance that they would die before we got to the second stage operation,” said Dr. Thomas Zellers, an interventional cardiologist at Children’s Health. He specializes in caring for newborns, children, and adults with congenital heart disease, and was called the “Godfather of Safe at Home,” at the Expo.
Zellers said these patients are born with conditions in which they only have one ventricle that pumps blood to their body. A Norwood operation creates blood flow through the lungs and into the body using the single ventricle.
The mortality rate has gone down significantly since the Safe at Home program has been in place.
“We’ve cut the mortality to 1.7 percent or less,” he said. “That’s about a tenfold decrease in patient mortality.”
They’ve accomplished that by giving parents 24/7 access to professionals as well as educating them about what they need to look for as far as the risk factors for their child having an adverse event and requiring hospitalization, or being at risk for death.
But Zellers said 1.7 percent is not not low enough.
“Our goal is to drive it as close to zero as we possibly can,” he said.
Other programs within the Heart Center also showed how their technologies and expertise are saving lives:
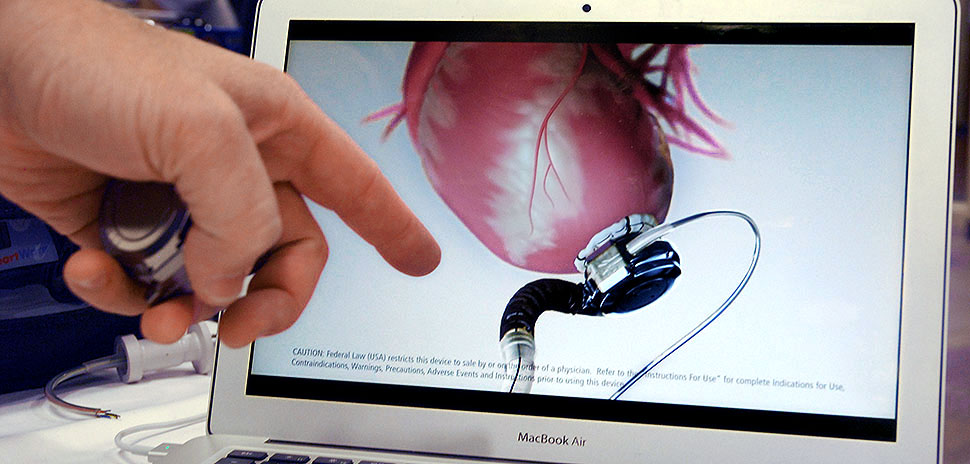
VENTRICULAR ASSIST DEVICES
Children’s Health is home to the only Ventricular Assist Device program for children in North and Central Texas, helping to ease the lives and outcomes for children with end-stage heart failure. Because of Children’s elite standing in the field, its physicians are among experts who participate in many international publications that are prominent in VAD clinical care.
A ventricular assist device is an implantable mechanical pump that supports the failing heart by pumping blood from the ventricles to the patient’s body. In children, it is a lifesaving tool that allows for possible recovery, transplantation, or a better quality of life.
“A lot of time and a lot of money goes into the development of these products.”
Dr. Vasiliki Vivian Dimas
Pediatric Cardiologist Dr. David Sutcliffe said the devices currently are too big to be used in very small children, but that efforts are ongoing to downsize the devices even more.
The Expo provided an opportunity for visitors to get a look at the Impella device — the world’s smallest heart pump. Dr. Vasiliki Vivian Dimas is leading the center’s use of and research related to the device.
“A lot of time and a lot of money goes into the development of these products,” Dimas said about the Impella and other interventional tools.
The Impella is a vascular assist device that is typically used in adults, but Dimas is leading efforts at Children’s Health to determine the effectiveness of the device in helping children with serious heart disease make it to transplant.
The device doesn’t require major invasive surgery and is inserted into the heart via an artery in the leg. The catheter pulls blood from one of the heart’s ventricles into the aorta allowing the heart to pump blood.

Dr. Vasiliki Vivian Dimas (center) explains how the Impella heart pump works to Katie Whitton, director of marketing and communications for the Southwest Transplant Alliance, while Dr. Alan Nugent listens. [Photo: Lance Murray]
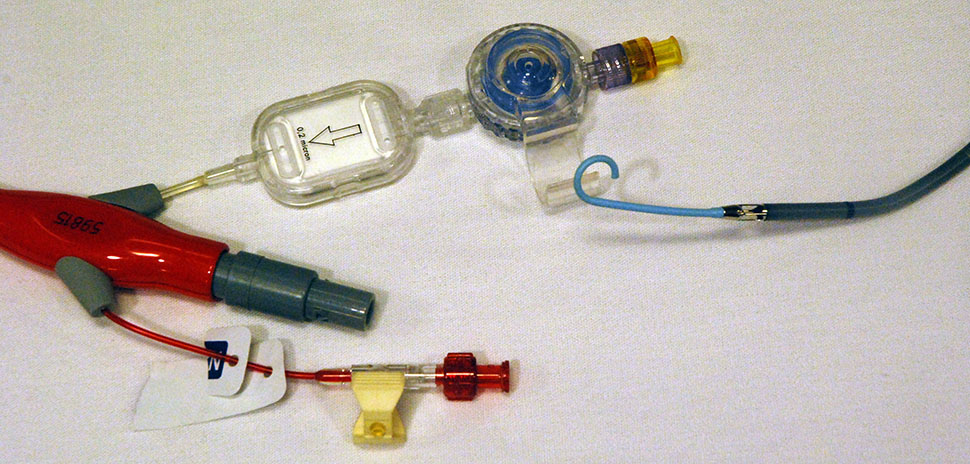
The Impella device is the world’s smallest heart pump and Dimas is leading an investigation into the device’s use to help save children with heart conditions at Children’s Health in Dallas. [Photo: Lance Murray]

Dimas shows the Impella device, the world’s smallest heart pump, during the Innovation Expo at Children’s Health. [Photo: Lance Murray]

Dimas (center) explains how the Impella heart pump works to Whitton during the Children’s Health Innovation Expo featuring the system’s Heart Center. [Photo: Lance Murray]
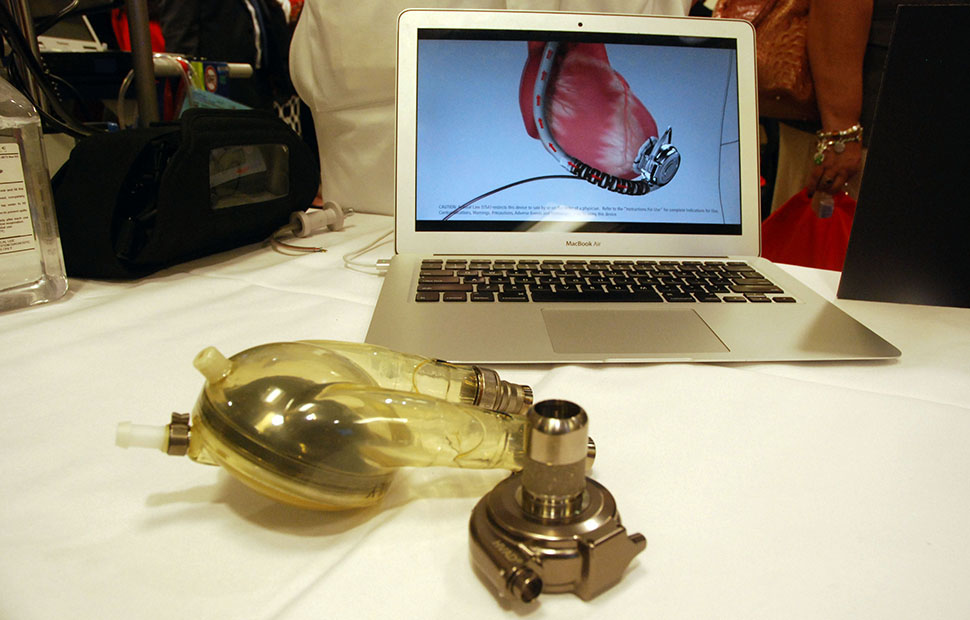
Long used in adults, Children’s Health is leading pioneering efforts that are making VADs available for use in smaller, younger patients. The current device ( show at right) is much smaller than a previous VAD next to it. [Photo: Lance Murray]

Dr. David Sutcliffe shows off the HeartWare ventricular assist device’s power unit. [Photo: Lance Murray]
3D HEART MODELS AND HOLOGRAPHIC DISPLAY TECHNOLOGY
Advanced imaging techniques are helping the Heart Center at Children’s Health evaluate, diagnose, and treat its pediatric heart patients.
The Children’s team uses state-of-the-art patient-specific imaging techniques to create 3D printed and interactive virtual models of the patient’s heart and the system’s pediatric cardiologists are developing software to help educate families through holograms and virtual reality models.
The 3D models are created using high-quality images of the heart via cardiovascular MRI, cardiovascular CT, or echocardiography scans. Doctors use dedicated software to show those images in a 3D format, which are converted into a virtual 3D image or a physical 3D model.
Doctors then use the 3D printed model to plan treatment procedures and show families what will happen in a 360-degree format. The models can later be used for medical training.
In preparation for complicated surgeries, holographic images are created and displayed, and physicians wear 3D glasses to study the hologram and get a precise understanding of the specific heart’s anatomy.

Sarah Stewart of Mended Little Hearts uses a VR headset to view a 3D tour of the heart that is shown on the screen behind her during Children’s Health’s Innovation Expo. [Photo: Lance Murray]

Stewart gets instructions from Dr. Animesh Tandon as she operates a virtual reality program. [Photo: Lance Murray]

Dr. Mohammad Hussain shows a 3D-printed rendering of a child’s abnormal heart to Jennifer Prinz and Sarah Stewart of Mended Little Hearts [Photo: Lance Murray]

A 3D-printed rendering of a child’s abnormal heart allows doctors to physically see an organ before they might operate on it. [Photo: Lance Murray]
EXTRACORPOREAL MEMBRANE OXYGENATION (ECMO)
Children’s Health has treated more than 760 children in life-threatening situations with the ECMO device in the past 25 years — more than any other program in North Texas.
It’s the last line of care when other treatments haven’t been successful, and it uses an artificial heart-lung machine to take over the work for the heart and lungs.
“It only allows the heart and lungs to rest,” ECMO team lead Donna Taylor said.
Here’s how it works:
The ECMO machine takes the blood without oxygen (so-called blue blood) from the right side of the heart and pumps it through an artificial lung — the oxygenator. Then, it’s warmed before the “red” blood is returned to the patient’s body.
ECMO team members are specially trained pediatric coordinators, surgeons, nurses, and respiratory therapists. They’re available 24/7 and Children’s said the equipment can be ready for a patient in 20 to 30 minutes. Children’s has nearly doubled its ECMO services in recent years and has been designated as a Center for Extracorporeal Life Support Organization.
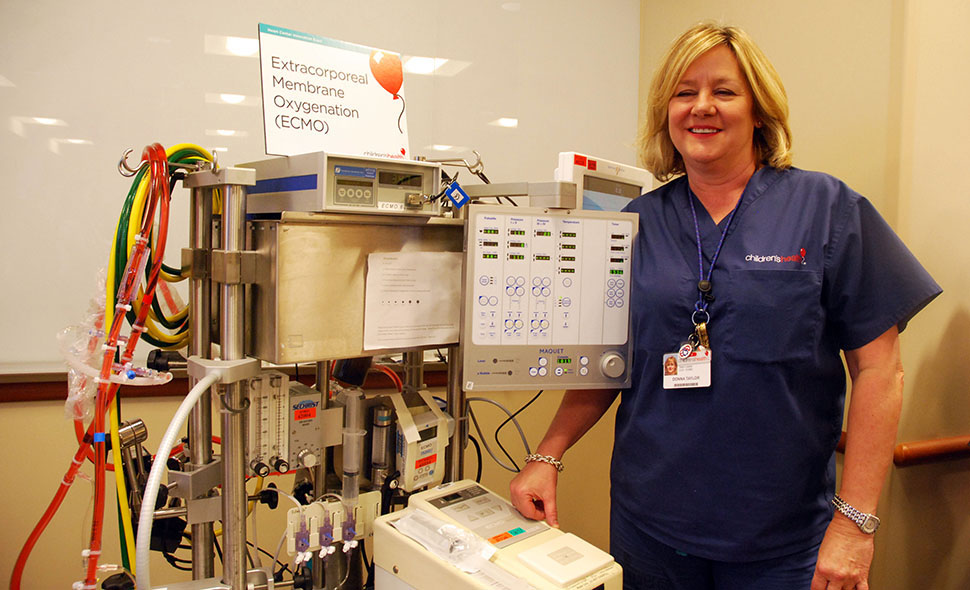
Donna Taylor shows off the ECMO machine during the Children’s Health Innovation Expo. [Photo: Lance Murray]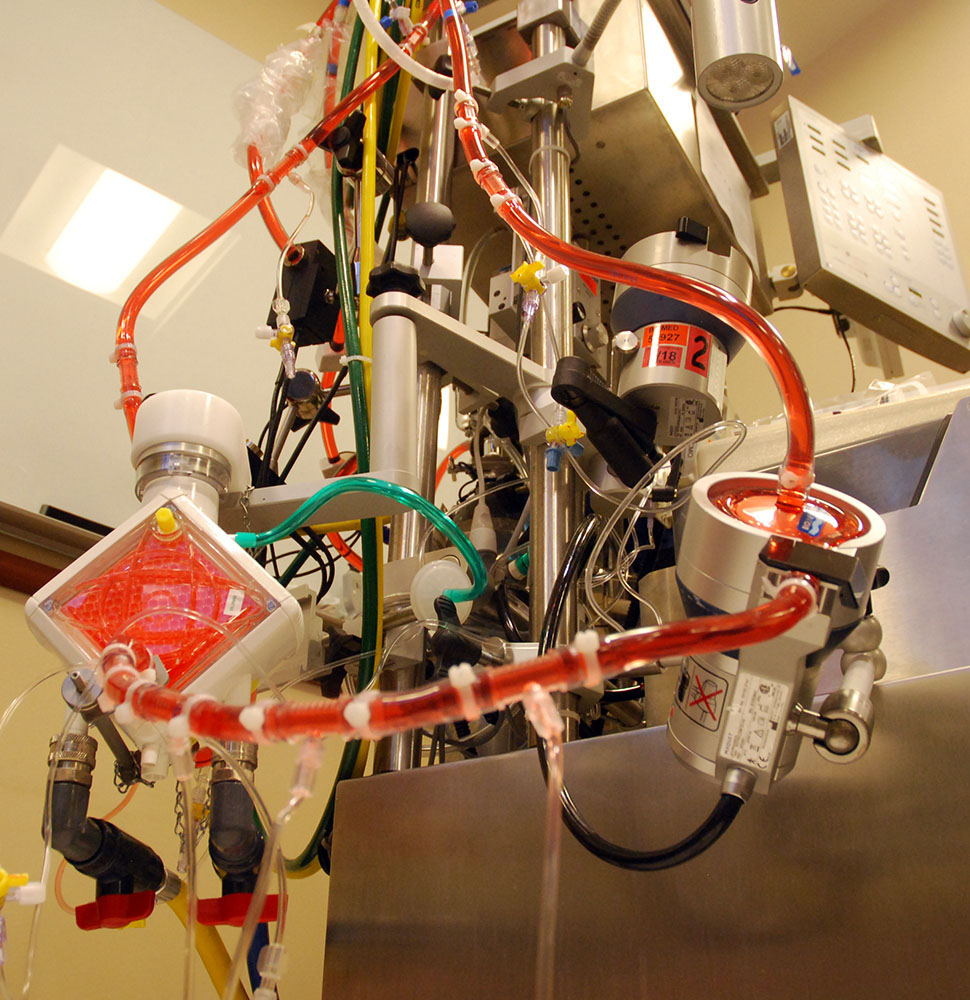
Tubing snakes up the side of an Extrocorporeal Membrane Oygenation machine which uses an artificial heart-lung machine to take over the work of the heart and lungs for someone who is in life-threatening condition. [Photo: Lance Murray]
CONGENITAL CORONARY ANOMALY PROGRAM
The Heart Center’s new Congenital Coronary Anomaly Program specializes in the diagnosis and management of congenital anomalies that, while rare, are the second-leading cause of cardiac deaths among youth athletes.
Congenital anomalies affect roughly 1 percent of the population, but they can have devastating and sometimes deadly effects on young athletes. The program focuses efforts on diagnosing and managing the effects of the anomalies allowing the young athletes to continue to safely compete in sports.
Nurses, sonographers, cardiologists, and surgeons comprise the program’s team which uses advanced testing to completely evaluate a patient’s heart health. The team works with the patient and parents to manage the condition to help avoid a life-threatening cardiac event.

Meredith Ford O’Neal (left) talks with Drs. Poonam Thankavei {center) and Adrian Dyer in front of imaging videos done as part of the Congenital Coronary Anomaly Program. Congenital coronary anomalies in the heart’s arteries, while rare, are the second-leading cause of cardiac death in young athletes. [Photo: Lance Murray]
INTERVENTIONAL CATHETERIZATION
The Heart Center at Children’s Health is one of the premier facilities in the world where interventional cardiologists use every test and procedure for the treatment of pediatric heart disease.
It’s also one of the world’s top cardiac cauterization programs, performing nearly 1,000 procedures each year. The center also began using groundbreaking techniques to become the first hospital in Texas to offer radiation-free catheterization using magnetic resonance imaging
![]()
Get on the list.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.
And, you’ll be the first to get the digital edition of our new Dallas Innovates magazine:
The annual edition publishes in January.