Two North Texas scientists are collaborating on research that might help determine whether a newborn baby is at risk of a condition that could lead to long-term health issues and disabilities.
The team includes a clinical translational intensivist at the UT Southwestern Medical Center in Dallas and a bioengineering professor at the University of Texas at Arlington.
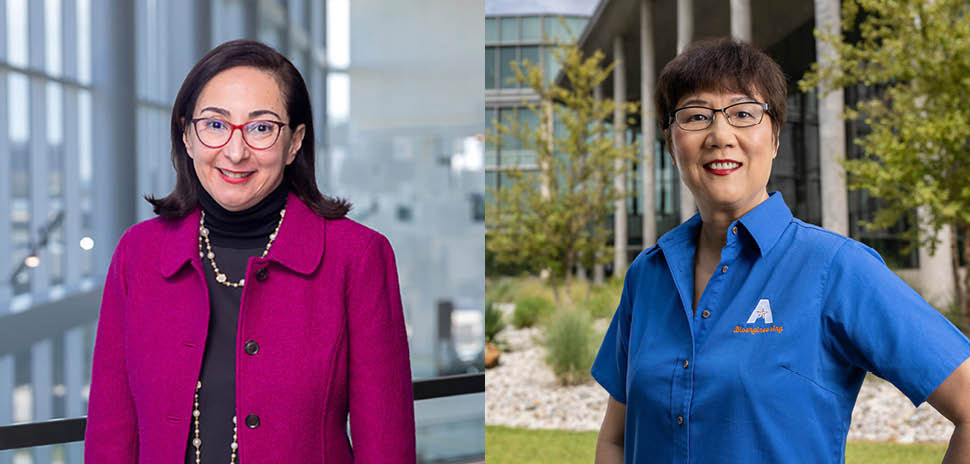
Dr. Lina Chalak, professor of pediatrics and psychiatry and interim chief of the Division of Neonatal-Perinatal Medicine at UT Southwestern, is principal investigator on the project. Chalak is founder and medical director of the Fetal Neonatal Neurology Program at UT Southwestern.
The National Institutes of Health funded the project with a $580,000 grant that flows through UT Southwestern.
Hanli Liu, a UT Arlington bioengineering professor, is working on a mathematical analysis that can help determine when a baby is at risk of hypoxic-ischemic encephalopathy (HIE), which occurs when oxygen or blood flow to the brain is reduced or stopped at birth.

The Hanli Liu lab at UT Arlington [Photo: UTA]
Brain condition in infants can cause cerebral palsy and other disorders and disabilities
HIE can cause cerebral palsy, intellectual disabilities, behavioral disorders, hearing impairments, visual disabilities, speech disorders, motor deficits, developmental disabilities, and seizure disorders, according to UTA.
“The brains of babies are very fragile and change dynamically at this time,” Lui, who holds the College of Engineering Board of Advisors Endowed Professorship at UTA, said in a statement. “If doctors can protect the little brains of those babies who need treatment, they recover. If not treated on time, the babies can sustain permanent brain damage. However, we aren’t sure right now which babies can recover and which ones can’t. That’s what we’re after, acquiring that information that shows which babies are in trouble.”
New approach aimed at better outcomes
Liu’s research is a novel engineering approach based on time-frequency analysis to look at how neuronal activity interacts with oxygen molecules in the blood of the brain at various times. Any inactive interaction between them gives a forecast of brain malfunctions and potential damage, the university said.
Chalak said that treatment strategies depend on the severity of the condition, the timing of intervention, and the individual situations of each baby.
Liu equated detecting HIE early to detecting COVID or cancer early because early treatments lead to more effective outcomes.
“But if we wait until the early or mild stage progresses to a moderate or severe stage of HIE,” Liu said, “then it’s more problematic to reverse the damage to the brain, leaving life-long damage to those with delayed treatment.”
Scientists have worked on the project since 2017
Liu has worked with Chalak, a physician-scientist whose research is focused on improving outcomes of the neonatal brain with HIE, on this project since 2017.
UTA said the just-funded $580K NIH grant is a competitive renewal of the one in 2017.
“We have had a very successful collaboration with excellent UTA bioengineering students working closely with my clinical team, leading to the success of another five-year NIH funding,” Chalak said.
“The project could save newborns’ lives, and the heartache that such sickness brings the babies’ family members and friends,” said Michael Cho, UTA’s Alfred R. Potvin and Janet H. Potvin Endowed Chair in Bioengineering.
Cho said Liu’s alliance with UT Southwestern’s Chalak’s shows a perfect example of how bioengineers help medical professionals develop improved medical devices or methodologies for prompt and efficient treatments.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.