Dallas-based American Heart Association (AHA) awarded more than $14 million in scientific research grants for health technology solutions focused on heart and brain health, including special projects related to COVID-19, last week. The grants went to four multidisciplinary teams around the country to create the AHA’s 10th Strategically Focused Research Network. The newest network centers on Health Technologies and Innovation.
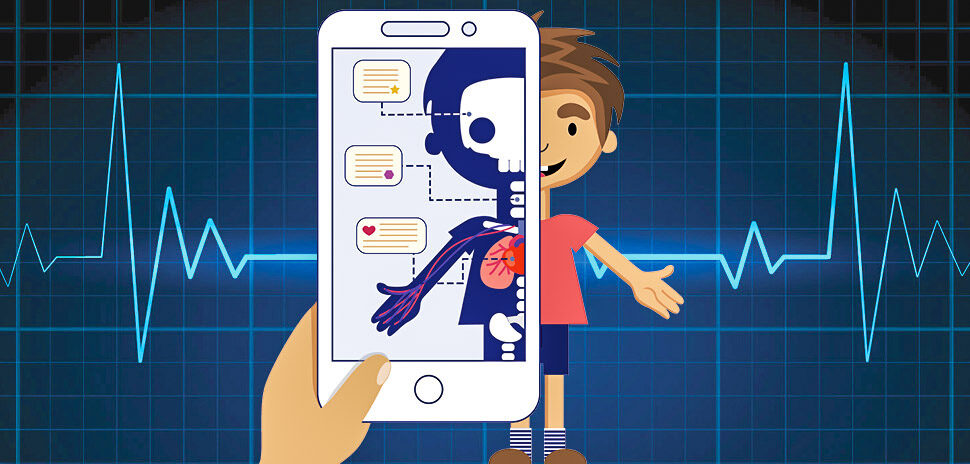
Consumer adoption of healthcare technology on digital mediums like tablets, smartphones, and wearable devices offer a “unique outlet to find new solutions to improve health outcomes,” American Heart Association president Robert A. Harrington said in a statement.
The AHA peer review team moved forward with its selection of the centers for its latest “strategically focused research network” when the COVID-19 pandemic in the U.S. broke. The nonprofit science-based organization knows the times are challenging as it works towards its mission of a culture of health.
“It felt this was an incredible opportunity for us to provide additional support in harnessing new innovations to tackle the challenges that are crippling the nation, and frankly the globe,” Harrington said.
Grantees that will create the 10th network are research teams at Cincinnati Children’s Hospital, The Johns Hopkins University, Stanford University School of Medicine and the University of Michigan. Each team will “receive $2.5 million each for their individual projects aimed at reducing health care disparities, empowering people to better manage their health and wellness, and enhancing patient/provider connectivity,” the AHA said.
AHA research ‘think tank’ and rapid-action COVID-19 tech solutions
Collectively the teams will also receive $4 million to work on “at least one highly impactful project and form a national Health Technology Research Collaborative,” it said. “The Collaborative may ultimately serve as an American Heart Association research ‘think tank’ to assist with identifying, creating, testing and bringing to scale future innovative health technologies.”
In addition, each research team also can apply for “supplemental research grants of up to $200,000 for rapid action projects to develop technology solutions to address the COVID-19 pandemic,” the AHA said. Those projects might provide aid for health care systems, doctors or care providers, first responders, patients or consumers.
These supplemental grants are part of the AHA’s $2.5 million commitment to research efforts to better understand this unique coronavirus and its interaction with the body’s cardiovascular and cerebrovascular systems.
“The peer review committee has assembled an exceptional network to move this work forward and I want to recognize the dedication and commitment of that panel of many renowned experts,” Harrington said. “The Association uses an intense, multi-stage review process in selecting the centers for our focused research networks and we’re very appreciative of the committee members who lend their time and expertise to this critical process.”
The AHA program brings together basic, clinical, and population researchers with engineers, IT developers, policy leaders, health care clinicians and patients. That lets the teams improve existing technology, and also “identify new and innovative ways to put technology to work in addressing heart and brain health,” American Heart Association volunteer James A. Weyhenmeyer, Ph.D. said.
Weyhenmeyer is vice president for research and economic development at Auburn University and chair of the Association’s peer review team for the selection of the new grant recipients. “It’s especially important that all of these projects be focused with an equity-first lens to ensure our most vulnerable populations are being served,” he noted.
Current funding for AHA’s Strategically Focused Research Networks (SFRN)
The AHA is currently funding seven Strategically Focused Research Networks (SFRN) with focuses on Go Red For Women, Heart Failure, Obesity, Children, Vascular Disease, Atrial Fibrillation, and Arrhythmias & Sudden Cardiac Death. Three of AHA’s networks—Prevention, Hypertension, and Disparities—have been completed. Locally, the University of Texas Southwestern was a grantee in the completed Prevention SFRN.
With the launch of its newest network, the American Heart Association has invested more than $190 million to establish 12 SFRNs since the program was launched in 2010-2011. The idea behind the science networks is the collaboration of scientists to focus research to address key strategic issues that were identified by the AHA’s Board of Directors, in areas such as hypertension, women’s health, heart failure, obesity, children, vascular disease, atrial fibrillation, sudden cardiac death, and type 2 diabetes. Each established network centers around the understanding, prevention, diagnosis and treatment of a key research topic. Four to six research centers make up each network, AHA said, which brings together investigators with expertise.
More networks can be expected in 2020 and beyond, AHA said.
The latest projects funded by the $14.5 million in grants commenced on April 1. Here they are, per the AHA:
Active Detection and Decentralized Dynamic Registry to Improve Uptake of Rheumatic Heart Disease Secondary Prevention (ADD-RHD) at Cincinnati Children’s Hospital
Led by Andrea Beaton, M.D., a pediatric cardiologist at Cincinnati Children’s Hospital, this team will address the global health issue of rheumatic heart disease which affects more than 40 million people, most living in poor countries or poor areas in wealthier countries. The team will concentrate on getting more people living with rheumatic heart disease into guideline-based care — using technology to find more people with rheumatic heart disease, keep them in care and generate the investment case to scale up national rheumatic heart disease action plans in low-income countries. Additionally, they’ll be looking for early career doctors and scientists who want to help people get better care using technology and educate this next generation in solutions developed to improve global health in the future. The team consists of a collaborative with the Rheumatic Heart Disease Research Collaborative in Uganda (RRCU) including the Uganda Heart Institute, Children’s National Medical Center and the University of Washington in Seattle; the Cincinnati Children’s Digital Experience and Bioinformatics Centers; Northern Kentucky University’s Biostatistics Department, Health Innovation Center and Health Sciences Institute; REACH (a global technical organization in rheumatic heart disease) and an industry partnership with Caption Health. While the project and solutions will be made for people living in developing countries, the team hopes to learn a lot about how to help people have better health in the United States.
Center for Mobile Technologies to Achieve Equity in Cardiovascular Health at The Johns Hopkins University in Baltimore
Led by cardiologist Seth Martin, M.D., M.H.S., and neurologist David Newman-Toker, M.D., Ph.D., this team’s mission is to leverage mobile and wearable technologies to empower patients and clinicians, enhance the quality of care, increase value and improve the diagnosis and management of heart diseases and stroke. Early and accurate diagnoses are essential to ensure the appropriate delivery of guideline-recommended management to engage patients and their caregivers to achieve the best patient outcomes possible. The collaborative project will span the patient experience from diagnosis to management to improve patient care throughout the patient journey. Specifically, the team will develop and test a smartphone application for stroke diagnosis, following their experience with a goggle-based eye-tracking technology in the Armstrong Institute Center for Diagnostic Excellence. On the management side, the team will work on a virtual cardiovascular rehab that builds on their Corrie Health platform to empower patients in guideline-based prevention. Patients and their families from demographically diverse backgrounds will join as partners in the technology advancement process.
Center for Heart Health Technology (H2T): Innovation to Implementation at Stanford University
Led by Mintu Turakhia, M.D. M.A.S., Executive Director of Stanford’s Center for Digital Health, associate professor of medicine and a cardiac electrophysiologist at the VA Palo Alto Health Care System, the H2T Center’s mission is to rapidly develop technologies that address unmet needs for heart health, evaluate them quickly and then implement these solutions at scale. The team will address the issue of high blood pressure, which affects more than 115 million Americans and costs the U.S. health care system more than $22 billion each year. The team will develop a clinician- and patient-facing digital health system for semi-automated management and evidence-based titration of blood pressure medications. The app will be tested in a randomized trial conducted in Northern California and New Jersey in people of different races, educations, and backgrounds and in a population of gig economy workers (rideshare drivers), who can be at increased risk of heart disease.
Wearables In Reducing Risk and Enhancing Daily Lifestyle (WIRED-L) at the University of Michigan
Led by Brahmajee Nallamothu, M.D., M.P.H., a professor in the Division of Cardiovascular Diseases at the University of Michigan, this team plans to establish the Wearables In Reducing risk and Enhancing Daily Lifestyle (WIRED-L) Center dedicated to building and testing mobile health (mHealth) apps that leverage wearables like smartwatches to improve physical activity and nutrition in hypertensive patients. The apps will use “just-in-time-adaptive” digital interventions to deliver notifications to participants when they are most likely to be responsive using contextual information obtained from their devices. WIRED-L will enroll diverse communities that include African Americans and older adults rarely included in mHealth studies, to better close the digital divide between rich and poor. Additionally, WIRED-L will train a diverse and inclusive set of future leaders in mHealth through a highly integrated program that focuses on the key and complementary areas of clinical trials, data science, and health equity research.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.