More than 51 million Americans experienced chronic pain in 2021, according to the CDC. And the NIH estimates that 2.1 million people in the U.S. have ‘opioid use disorder.’ The founders of Dallas-based biotech startup Cacti don’t think that’s a coincidence.
Combining what they know about brain development and function, Kaitlin Roberson, CEO of Dallas-based Cacti, Inc., and David Roberson, Cacti’s lead scientific advisor, are taking a novel approach to treating chronic pain, by addressing the trauma that is often at its root.
“Cacti has two programs … one seeks to reset ‘angry’ pain nerves by delivering a psychedelic molecule directly to the nerve sending the pain signal. Essentially, we’re trying to make pain nerves trip,” said David. “And the other approach is a therapeutic catalyst: a psychedelic-derived medicine that targets the part of the brain that processes the emotional aspects of pain, which will be paired with psychotherapy to train the brain to process pain differently.”
To develop these new medicines, Cacti is using technology from Roberson’s company, Blackbox Bio.

David Roberson, PhD, MBA, founder of Blackbox Bio [Photo: Blackbox Bio]
AI-enabled drug development
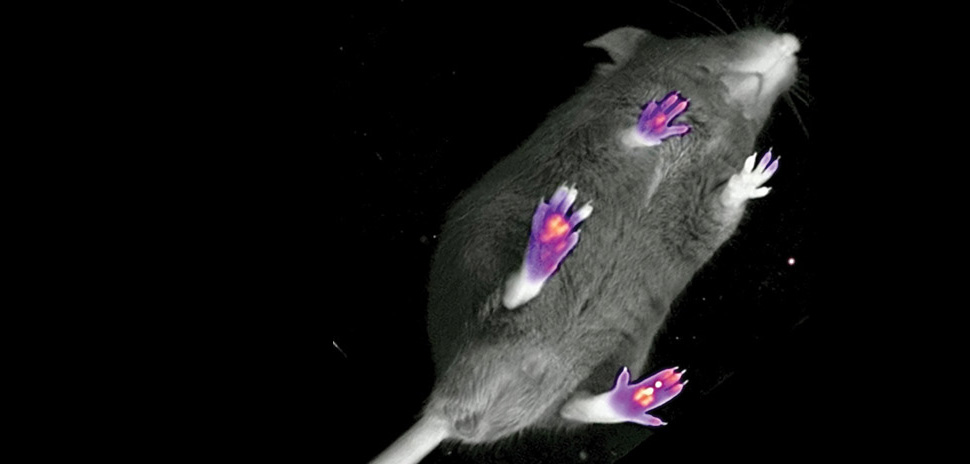
Also based in Dallas-Fort Worth, Blackbox Bio uses artificial intelligence to watch how lab mice and rats behave under different circumstances, such as when they have arthritis pain or when they’ve been given an experimental drug for their pain. The company’s scientific instruments observe the effect of a drug on rodents from below. This is important because prey animals, like mice and rats, have developed ways to hide injury and weakness from the view of predators for the purpose of self-preservation.
Watching from below allows their AI algorithms to see if the rodents are favoring a limb, struggling with balance, or even if they’re scared (they walk on their tiptoes). “Mice only live for about a year and a half. So, you can observe the effects of a drug over their whole lifespan; you can take a mouse that has experienced a stroke and test a new therapy to see how it affects the rest of their life, in a relatively short period of time,” he said.
Using this process improves the quality of the observational data and accelerates the steps needed to get a drug approved. “By using AI to watch mice instead of human observation, outcomes are better. As a result, fewer animals are needed and the results are more reliable,” said David. “The long-term goal of our technology is to use these rich data sets to generate AI virtual mice that will replace live lab animals in many cases.”
Cacti is using the Blackbox technology to identify new psychedelic-derived medicines but without the hallucinations and other side effects that classical psychedelics can cause. The device can look at a mouse and automatically tell if it is experiencing a psychedelic hallucination.
“Having access to this technology has given us a head start in our search for new therapies that can heal the root cause of chronic pain,” said Kaitlin.

Kaitlin Roberson, founder of Cacti [Image: Cacti]
Cacti begins to grow
But four years ago, in Massachusetts, before Cacti began the path toward FDA approval for its new medicines, the idea for the startup was just coming together.
It was 2020 and the Robersons (all six of them, plus their Vizsla, Ruby) were living in Harvard University housing, where Kaitlin was finishing her graduate program.
“We were living in a tiny little apartment right off Harvard Square,” Kaitlin said.
Picture one thousand square feet of apartment space with only one toilet; their oldest son was twelve years old; the twins were seven, and their younger sister was five.
And then COVID-19 shut the city down.
“I turned to David and I said, ‘I’m not worried about the virus at this point. But I do think we may die by our own hands,” she said.
They needed to get out of that apartment, but initially the plan wasn’t to leave the Bay State.“We’d been out in the Boston area for 11 years at that point and we were really happy there,” Kaitlin said.

The Roberson family. [Photo: Cassie Shaw Photography]
But they started thinking more holistically. David is a scientist and can work from anywhere, and Kaitlin had done a lot of work in the humanitarian field, mostly with the refugee population.
“And my thinking was, you know, why not move to a border state that is not only the largest refugee resettlement state in the country, resettling refugees from all over the world, but also a border state also contending with asylum seekers and immigrants,” said Kaitlin.
She took a job with a resettlement agency that has offices all over Texas, but it went bankrupt the following year.
Meanwhile, David — a neurobiologist and drug developer — had been toying with the idea of a startup that would integrate the use of psychedelics to treat chronic pain. Specifically, he was looking at phenethylamines, medicinal substances made by the cactus family.
“We started talking about combining our two areas of training and see if we could take an interdisciplinary approach to chronic pain,” she said.
Reinventing pain management
With her background in developmental psychology, Katilin assumed the role of CEO and Cacti—named in honor of the compound David had identified for development—was born.
Where traditional pain management has focused on treating the acute feeling and overlooked the psychology behind it, Cacti focuses on the experience of pain and how it correlates to brain function.
“Depression, grief, and other negative emotions are processed in the same part of the brain that gets activated when people have chronic pain,” said David.
Cacti wants to treat the trigger. The working theory is that just like emotions can resurrect a memory of mental pain, they can also remind the body of physical pain, keeping the sensation active.
“I think one of the things that is lacking in Western medicine is the connection between body and mind. And pain is treated in this very isolated way where it’s just a certain receptor being targeted,” said Kaitlin.
Cacti’s approach aims to bring together body and mind, by pairing psychedelics with psychotherapy – but a new model presents additional hurdles.
“So even when a new medicine does get approved, there’s still a question of how this treatment will fit into our health care system. With psychedelics, it’s like an eight-hour journey with the patient. Will insurance pay for the drug and the time spent with a therapist as it takes effect?”
A future without pain
Cacti’s medicines are not yet in human trials, but they are creating a treatment that would work for multiple communities of people who have trauma-triggered chronic pain, including the refugees to whom Kaitlin devoted her early career. “It’s a long road to FDA approval for a first-in-class medicine, but we’re committed to the patients with chronic pain who deserve more effective treatments, and we’re well on our way to finding them,” she said.
That means a future without Opioid dependence may be closer than you think.
Voices contributor Nicole Ward is a data journalist for the Dallas Regional Chamber.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.