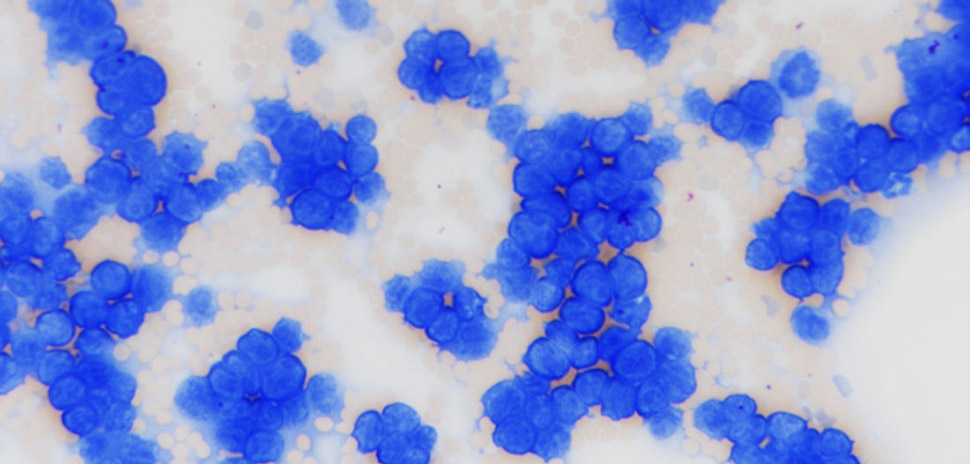
Existing treatments for leukemias and lymphomas can be effective. But for many people, they work only up to a point and may stop working altogether. That makes a new treatment option of paramount importance—and a research team at UT Southwestern in Dallas may have just found a big lead.

Jin Huk Choi, Ph.D.
By targeting a protein called ZFP574, the team was able to suppress leukemia in a mouse model of the disease. Their findings could lead to new treatments for leukemias and lymphomas in human cancer patients.
Jin Huk Choi, Ph.D., assistant professor in UTSW’s Center for the Genetics of Host Defense and of Immunology, noted that effective treatments exist for B-cell malignancies such as leukemias and lymphomas.
“But in a significant portion of patients, these treatments stop working and their disease recurs, leaving them with no viable treatment options,” Choi said in a statement. “Targeting ZFP574 could eventually fill an unmet need, either as a primary or backup therapeutic.”
The scientists’ research was funded by the National Institutes of Health, UTSW said.
Choi co-led the study with a Nobel Prize winner
Bruce Beutler, M.D.
Choi co-led the study with Bruce Beutler, M.D., director of the Center for the Genetics of Host Defense and professor of immunology and internal medicine at UTSW. Their findings were published in PNAS (Proceedings of the National Academy of Sciences).
Dr. Beutler shared the 2011 Nobel Prize in Physiology or Medicine for his discovery of an important family of pathogen sensors known as Toll-like receptors found on immune cells.
The study’s first author is Xue Zhong, Ph.D., an instructor in UTSW’s Center for the Genetics of Host Defense and of Immunology. Drs. Choi and Zhong are former postdoctoral researchers in the Beutler Lab at UT Southwestern.
UTSW said that Beutler has long used mutagenesis—introducing mutations into the genes of animal models through exposure to a chemical called N-ethyl-N-nitrosourea—as a key tool for discovering how genes function. The Beutler Lab recently pioneered a method known as “automated meiotic mapping” to trace unusual features in mutant mice. That helps to identify genes that are needed to maintain normal physiology.
When the team combined these techniques in mice, they searched for genes that might play key roles in the development of B cells—white blood cells that fight infections as part of the adaptive immune system.
Zeroing in on the Zfp574 gene

Xue Zhong, Ph.D.
The team quickly zeroed in on a gene called Zfp574, which produces the ZFP574 protein—something that hadn’t previously been known to have an immunity function.
Their experiments showed that mutating this gene in embryos prevented development, suggesting that the gene is essential to life. “When the researchers used a genetic technique to control its activity in healthy adult mice, they found that switching Zfp574 off dramatically decreased the number of B cells, making the animals immunodeficient. Further experiments showed that ZFP574 appears to be responsible for controlling an important part of the cell cycle, the process by which cells multiply,” UTSW said.
‘Inhibiting the cell cycle’ to treat leukemia and lymphoma
Many cancer drugs work their wonders by inhibiting the cell cycle, UTSW noted—preventing malignant cells from performing their usual rapid division. So the research team decided to explore whether inhibiting ZFP574 could treat B-cell cancers such as leukemia and lymphoma.
When they performed tests in a mouse model of leukemia, results were striking. Mutating or deleting Zfp574—or simply using pharmaceuticals to degrade it—”reduced the amount of malignant B cells by as much as 92%,” UT Southwestern said.
Normal B cells were largely spared, since their cell division happens significantly more slowly, according to Choi.
Beutler: ‘Perhaps many cancers’ will respond to this treatment
“Not only leukemias and lymphomas, but perhaps many cancers will respond to inhibition of ZFP574,” said the Nobel Prize-winning Beutler, a member of the Cellular Networks in Cancer Research Program in the Harold C. Simmons Comprehensive Cancer Center at UT Southwestern. “The use of a random germline mutagen to discover a new and essential component of the cell cycle—despite the fact that the cell cycle has been intensively studied for many years—suggests there may still be plenty of new targets to exploit in controlling cancer cell proliferation.”
UT Southwestern said that future studies will focus on ZFP574’s atomic structure and how it controls B-cell cycling—potentially helping pharmaceutical companies develop drugs that could target ZFP574 to treat leukemias, lymphomas, and other cancers.
Other UTSW researchers who contributed to the study are James J. Moresco, Ph.D., Assistant Professor in the Center for the Genetics of Host Defense and of Biophysics; Jeffrey A. SoRelle, M.D., Assistant Professor of Pathology and Pediatrics; Eva Marie Y. Moresco, Ph.D., Assistant Professor in the Center for the Genetics of Host Defense and of Immunology; Ran Song, Ph.D., Mylinh T. Nguyen, M.S., and Jianhui Wang, M.S., Senior Research Scientists; Chun Hui Bu, Ph.D., Computational Biologist; and Yiao Jiang, Ph.D., postdoctoral researcher.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.