![]() Every week, we do a little research of our own. We’re looking for scientists, professors, engineers, entrepreneurs—anybody, really—engaging in research and development across North Texas.
Every week, we do a little research of our own. We’re looking for scientists, professors, engineers, entrepreneurs—anybody, really—engaging in research and development across North Texas.
There’s plenty of good work being done. If you want to put R&D under your microscope, sign up for our e-newsletter.
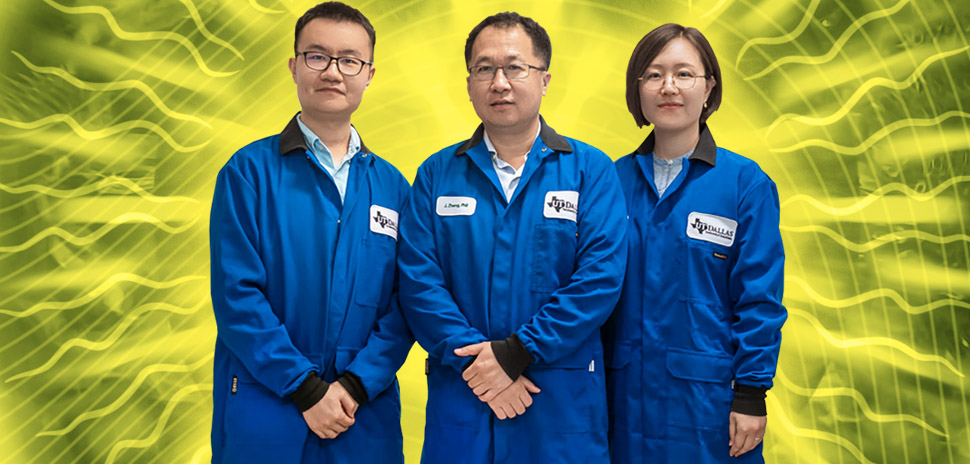
UTD team reveals how to make nanomedicines safer to use
Research into the use of nanomedicines has been going on for a long time, but a team at the University of Texas at Dallas has recently shown that they can improve the interactions of nanomedicines with the liver, while minimizing side effects.
UTD chemistry professor Jie Zheng, thinks he’s “turned a barrier into a bridge” in the use of nanomedicines, according to a statement.
“People have been working on nanomedicine for decades. It has great potential to advance cancer treatment and detection.”
Jie Zheng
Zheng and his UTD research team at UTD have shown that nanomedicines can be designed to interact with a natural detoxification process in the liver to enhance their disease targeting and lessen potential side effects.
“People have been working on nanomedicine for decades. It has great potential to advance cancer treatment and detection,” Zheng, the Cecil H. and Ida Green Professor in Systems Biology Science in the Department of Chemistry and Biochemistry at UTD, said in a statement. “But there are potential hazards as well.”
The researchers’ major discovery—conducted in a mouse model—is that one of the liver’s natural toxin-removal processes can be used to enhance the delivery of nanomedicines while also making them safe.
Nanomedicine—the use of engineered nanoparticles, defined by their microscopic dimensions— is employed for a variety of health-related reasons. It can help pinpoint the delivery of drugs and detect various diseases. As the biggest detoxification organ in the body, the liver captures and removes many substances that originate inside or outside the body.
“The liver protects us every day from damage from foreign materials,” Zheng said. “But it is also a long-standing barrier to making safe and effective nanomedicines that patients can use.”
Even though many nanomedicines target diseases efficiently in preclinical studies, Zheng said that not many reach clinical use because a type of white blood cell in the liver called macrophages capture and store nanomedicines in the body long term, lowering their effectiveness and increasing their toxicity.
“The challenge is maximizing their treatment potential while minimizing side effects,” he said.
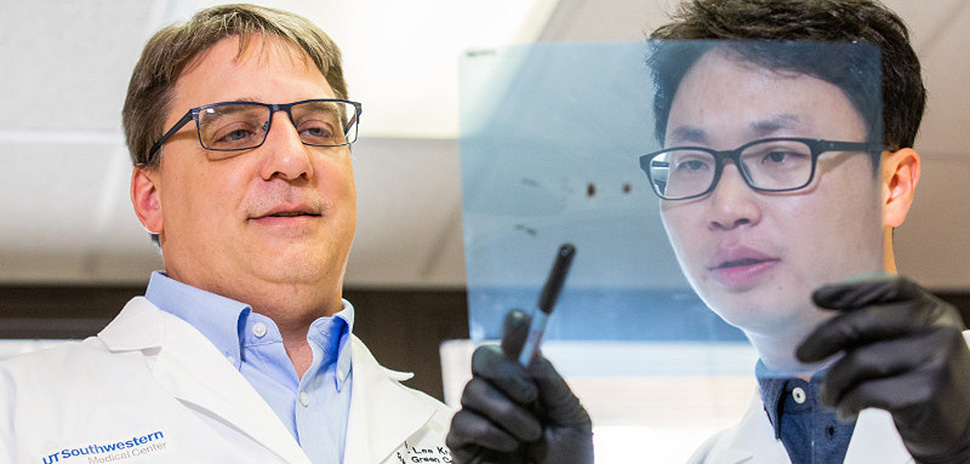
Dr. W. Lee Kraus with Dr. Dae-Seok Kim in the lab at UT Southwestern Medical Center. [Photo: Courtesy UT Southwestern]
UTSW team makes discovery in use of PARP inhibitors against cancers
Researchers at UT Southwestern Medical Center in Dallas have discovered that a new molecular mechanism indicates drugs used to treat a small number of breast cancer patients—known as PARP inhibitors—might have broader effectiveness in treating all cancers where they are used.
Ovarian and prostate cancers are among the diseases that the drugs may be used to treat, according to UTSW. The researchers also showed a potential biomarker indicating when these drugs—currently used for 10 percent of breast cancer patients—can be engaged in fighting cancer.
“These findings could increase the patient population benefiting from these drugs by two, three, or four-fold. Up to 70 percent of breast cancer patients could now be good candidates,” W. Lee Kraus, director of the Green Center for Reproductive Biology Sciences at UTSW, said in the statement. “We have found that PARP inhibitors can act by a mechanism that is different from those previously identified, which rely on BRCA-dependent DNA repair pathways.”
This information helps explain why breast cancer patients can be responsive to PARP inhibitors even if they don’t have BRCA gene mutations. PARP inhibitors were approved in 2014 by the FDA to treat ovarian cancers containing BRCA mutations, which are rare genetic mutations that disable DNA repair pathways in cancer cells.
The FDA approved PARP inhibitor use for breast cancer treatment last year. Doctors currently prescribe PARP inhibitors to disable a second DNA repair pathway, making it harder for cancer cells to survive.
UTA researcher gets $634K grant to study T cell role in cardiovascular disease
What role do T cells play in cardiovascular disease in older people?

Daniel Trott
Daniel Wayne Trott, a researcher at The University of Texas at Arlington’s College of Nursing and Health Innovation, will use a $634,000 National Institutes of Health grant to try to answer that question about T cells, one of two types of lymphocytes that determine the immune response to foreign substances in the body.
The five-year NIH grant awarded to Trott, an assistant professor in the Department of Kinesiology, is a career development award known as a KO1 grant. The grant is designed to give enhanced mentoring for promising junior faculty to learn techniques that will increase their research profiles.
Trott will be mentored by three nationally-renowned cardiovascular scholars on this study: Paul Fadel, a UTA professor of kinesiology and the college’s associate dean for research; Tony Donato, an associate professor at the University of Utah’s School of Medicine; and Jorg Goronzy, a professor of medicine at Stanford University in California.
Age is the most predictive factor of cardiovascular disease, Trott said in a statement, and his preliminary research shows that T cells infiltrate arteries in pre-clinical models.
“These studies are designed to give us an answer as to whether this occurs in older adults,” he said. “We know there is an increased risk for cardiovascular disease with aging. We think that aging T cells may be involved in this increased risk.”
The work builds on Trott’s efforts as the principal investigator of the college’s Integrative Immunology Laboratory that focuses on finding out how the immune system and arteries interact in older people, according to UTA.
One aim of the the grant is to help train Trott in performing clinical human research. Next year, Trott and his team are expected to start recruiting 54 people for the study who fall into the age categories of 18-30, 35-50, and 55-75.
2 UTD scientists receive honors for their work

Michael Burton

Jenny Boothby
On the accolades front, two researchers at the University of Texas at Dallas have been honored for their work.
Dr. Michael Burton, an assistant professor in the School of Behavioral and Brain Sciences, has received the 2019 Mitchell Max Award for Research Excellence from the National Institutes of Health Pain Consortium.
He was chosen based on his presentation on delayed-onset neuropathic pain in older men. Burton’s work suggests that immune system hyperactivity at an advanced age can cause hyperexcitability in neurons, producing chronic pain long after an injury.
Jennifer Boothby, a biomedical engineering doctoral student at UTD, was awarded a highly competitive silver award from the Materials Research Society at the organization’s spring meeting in Phoenix, Arizona.
Boothby was one of 13 students that received the silver award from the society, which is regarded as the premier professional organization for materials scientists. It presents gold and silver awards to graduate students at its annual spring meeting.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.