Researchers at the University of North Texas and Stanford Medicine say they have created the first mini hearts and livers with complete blood vessel networks. The stem cell–based breakthrough could make lab testing safer, reduce reliance on animal models, and advance heart disease research.
The findings, published in Science, come from a project co-led by Adam (Huaxiao) Yang, assistant professor in UNT’s Department of Biomedical Engineering, and Dr. Oscar Abilez of Stanford Medicine, with contributions from Rosebud Biosciences, Bullseye Biotechnologies, and Greenstone Biosciences.
Why it matters
Organoids are tiny lab-grown versions of real organs. Without blood vessels, they can’t grow beyond a small size or function like real tissue.
Yang and Dr. Joseph Wu at Stanford Medicine say they are the first to grow mini hearts and livers with fully formed, self-organizing vessel networks. That makes them more realistic and useful for studying diseases and testing treatments. Wu is director of the Stanford Cardiovascular Institute and the Simon H. Stertzer, MD, Professor of Medicine and Radiology.
From concept to breakthrough
Yang began the vascularized organoid work in 2017 at Stanford and continued it after joining UNT in 2020. His team grew the organoids from pluripotent stem cells, guiding them to form multiple heart and liver cell types, including the cells that create blood vessels.
According to Stanford, the researchers tested 34 variations of growth factor “recipes” before finding one that produced strong vessel networks and nearly all the cell types found in a six-week-old embryonic human heart.
“It really is groundbreaking because no other work before has built a fully vascularized network in the heart and liver organoids,” said Angello H. Gomez, a UNT Ph.D. student who led parts of the project.
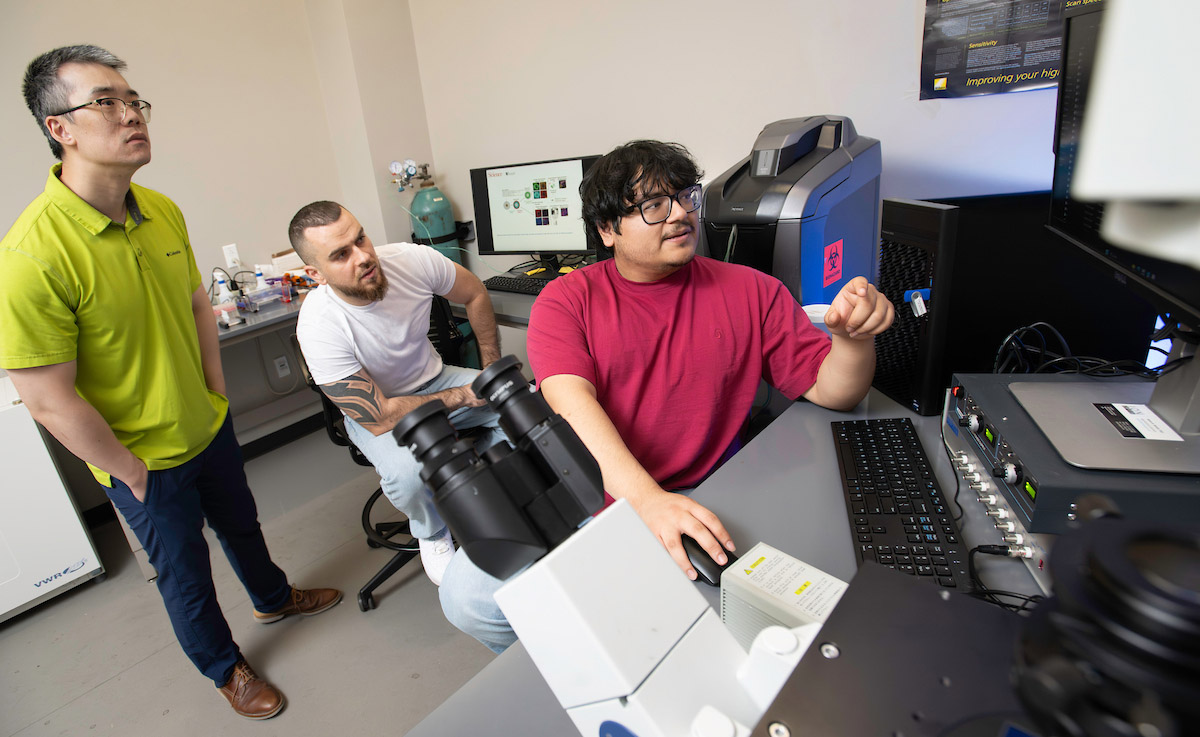
Adam Yang with Ph.D. students Marcel El-Mokahal and Angello H. Gomez. Yang, assistant professor in the College of Engineering’s biomedical engineering department, and his team are creating tiny lab-grown artificial organs called organoids in his independent lab. [Photo: UNT]
Building on the discovery
The organoids are about 2 millimeters in diameter and mimic an early-stage human heart. Yang and Gomez say the method could bridge engineering and biomedical research, providing cardiologists and drug developers new tools for early testing.
“These organoids can become an alternative to animal models,” Yang said, noting that the FDA’s Modernization Act 2.0/3.0 supports organoid use for drug and genetic disease testing when possible.
For Gomez, the work is personal. “I had a cousin who had congenital heart disease, and he didn’t make it,” he said. “I want to use my skills and knowledge and contribute to lowering cardiovascular disease.”
Gomez is now working on mimicking blood flow in the organoids to study heart development and potentially model congenital heart disease for drug or gene therapy research.
Stanford’s Abilez said vascularized organoids made from a patient’s own stem cells could one day connect to the body’s blood supply, improving survival if implanted.
“There’s so many applications for these vascularized organoids,” Gomez said. “I’m glad I can do my part.”
Don’t miss what’s next. Subscribe to Dallas Innovates.
Track Dallas-Fort Worth’s business and innovation landscape with our curated news in your inbox Tuesday-Thursday.

![Organoids without blood vessels can't grow larger than sesame seeds—about 3 millimeters—before dying from lack of oxygen and nutrients. UNT and Stanford researchers say they've solved this problem. Seeds pictured above are not to scale. [Image: Pinchai Puntong/istockphoto]](https://s24806.pcdn.co/wp-content/uploads/2025/08/Sesame-Seed-organoid-science-iStock-1487667097.jpg)