UT Southwestern Medical Center has landed up to $25 million from the Advanced Research Projects Agency for Health to pursue an ambitious goal: creating fully functional, patient-specific artificial livers that could ease the nation’s chronic organ shortage and reshape how liver disease is treated and studied.
The five-year project, known as Vascularized Immunocompetent Tissue as an Alternative Liver, or VITAL, aims to “biofabricate” livers using patients’ own cells and advanced 3D printing techniques. UT Southwestern said the approach could help reduce transplant waitlist deaths, eliminate the need for lifelong immunosuppression, and create new platforms for drug testing and liver disease research.
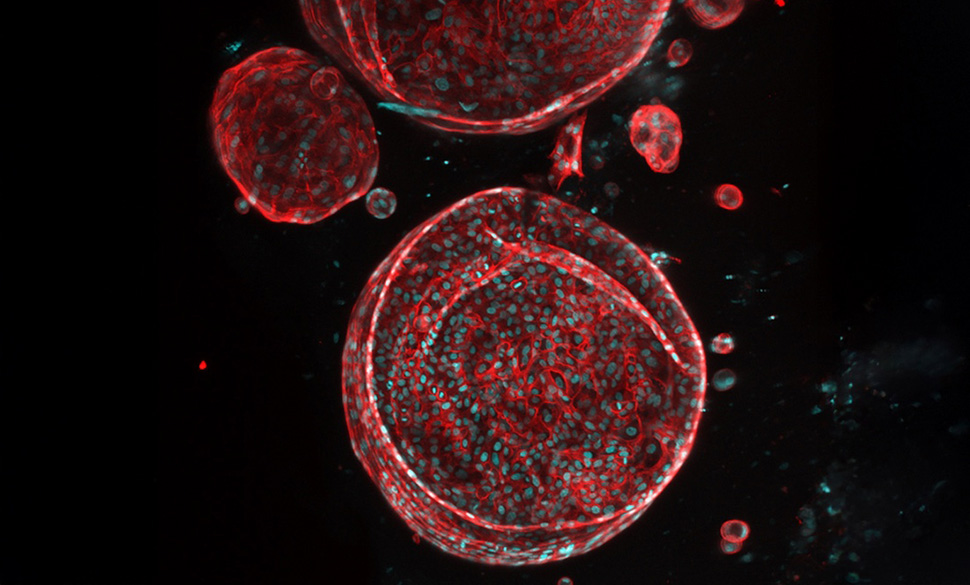
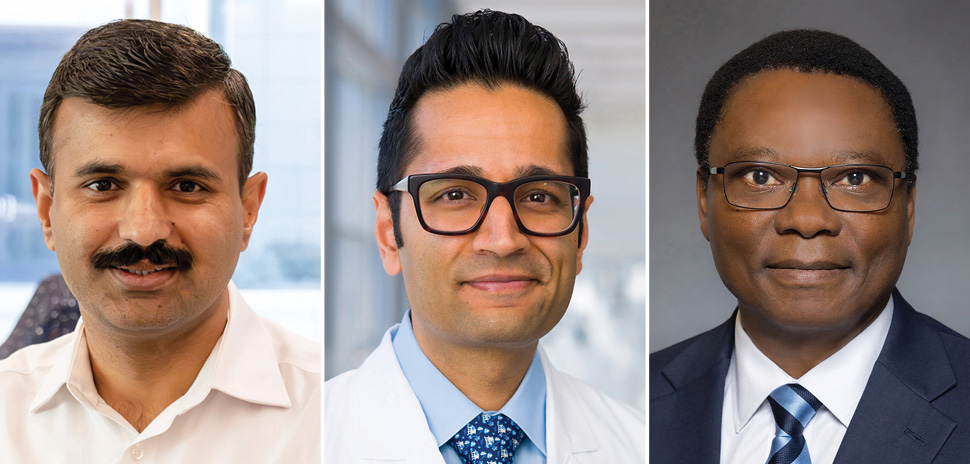
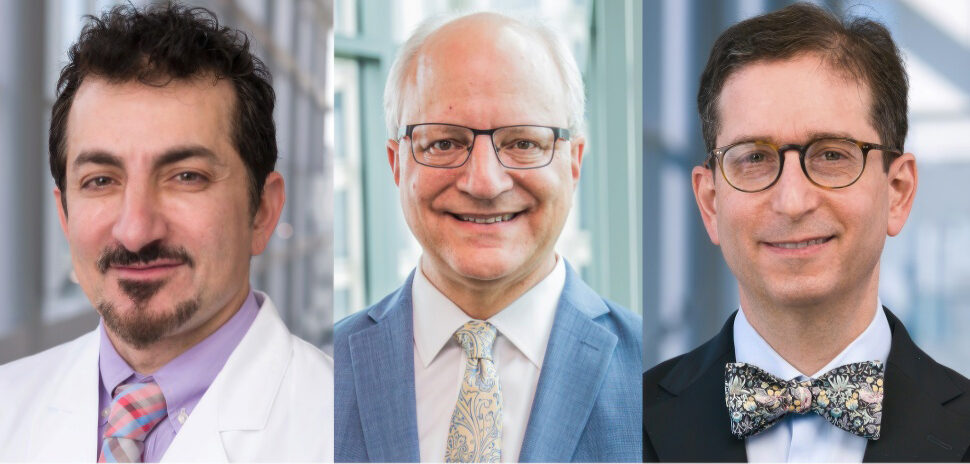
Image: UTSW
The work is funded through ARPA-H’s Personalized Regenerative Immunocompetent Nanotechnology Tissue program, which supports ambitious biomedical projects with long-term clinical and translational potential.
“Over the last two decades, researchers have made remarkable progress toward the goal of creating lab-made organs, including innovations in biomaterials, stem cell differentiation, and bioprinting,” Muhammad Rizwan, Ph.D., assistant professor of biomedical engineering and ophthalmology at UTSW and the project’s principal investigator, said in a statement. “UT Southwestern is an ideal environment to bring together the recent advances that have never been combined before.”
A persistent transplant gap
The stakes are high. Each year, liver cirrhosis and chronic liver diseases cause about 50,000 deaths in the United States. As of September 2024, nearly 10,000 people were waiting for a donor liver, with average wait times of about seven months, according to the Health Resources and Services Administration. Up to 31% of patients die while waiting.
Clinicians have tried to narrow the gap through strategies such as living donation and improved preservation of donor organs. Those efforts, however, have not solved the underlying shortage.
“Finding a way to generate artificial livers that function as well as natural ones could offer a solution,” said Madhukar Patel, M.D., M.B.A., Sc.M., assistant professor of surgery at UTSW and surgical director of its liver transplantation program. Artificial livers could also address other challenges associated with transplantation, including the need for lifelong immunosuppression and the high cost of liver transplants, which can approach $1 million, he said.
How the project works
Under the VITAL program, researchers will harvest cells from patients with liver disease and reprogram them into induced pluripotent stem cells, which can develop into any cell type in the body. Jun Wu, Ph.D., associate professor of molecular biology, will lead the effort to convert those cells into the range of cell types required to build a liver.
Those cells will be combined with a hydrogel “bioink” to enable three-dimensional printing of liver tissue that includes blood vessels and bile ducts, two structures that have limited previous attempts to scale lab-grown liver tissue into functioning organs.
Dr. Rizwan said his team has developed a novel approach that supports the growth of both blood vessels and bile ducts within engineered liver tissue, bringing the field closer to a fully functional artificial liver. As part of the effort, he is establishing a scalable organoid manufacturing facility at UT Southwestern.
The bioprinted livers will first be tested in small and large animal models, with potential testing in humans in about five years, Dr. Rizwan said. He estimates that a patient-specific liver could be generated in 10 to 13 weeks.
Because the organs would be created from a patient’s own cells, transplanted livers would not require immunosuppression, UT Southwestern said.
More than a transplant solution
The effort isn’t limited to organ replacement. Artificial livers could also serve as advanced platforms for evaluating drug safety and effectiveness and could help researchers better understand how the liver functions and fails in disease.
“This project represents a bold step toward advancing patient care through biomedical innovation,” said Samuel Achilefu, Ph.D., inaugural chair of biomedical engineering at UTSW and a co-investigator on the project. “It unites engineers, clinicians, and scientists to transform discovery into real-world solutions, shaping a future where functional organ printing becomes reality.”
Dr. Achilefu will use noninvasive imaging techniques to evaluate the performance of the bioprinted livers.
A collaborative North Texas effort
The project brings together researchers across UT Southwestern, including Hao Zhu, M.D., Walter Akers, Ph.D., D.V.M., and Yasin Dhaher, Ph.D., supported by 11 core facilities and the institution’s hepatology clinics. Collaborators from Pennsylvania State University and the University of California, Davis, will contribute expertise in three-dimensional printing technology and GMP cell manufacturing.
UT Southwestern said its integrated research and clinical infrastructure, including a solid organ transplant program that recently marked its 1,000th liver transplant, positions the institution to take on complex regenerative medicine efforts like VITAL.
The ARPA-H award provides up to $24.9 million over a 60-month period.
Don’t miss what’s next. Subscribe to Dallas Innovates.
Track Dallas-Fort Worth’s business and innovation landscape with our curated news in your inbox Tuesday-Thursday.