Joint replacements have given millions of people a new lease on life. But for a small percentage of them, a dangerous complication can arise. A Dallas biotech company is tackling a rare but serious infection that can have devastating consequences. And now it has raised $50 million in Series D funding to bring its lead drug and device combo to market.
Osteal Therapeutics, which relocated from California to Dallas about four years ago, is developing a groundbreaking treatment for periprosthetic joint infection (PJI), a condition where bacteria create stubborn “biofilms” on artificial joints.
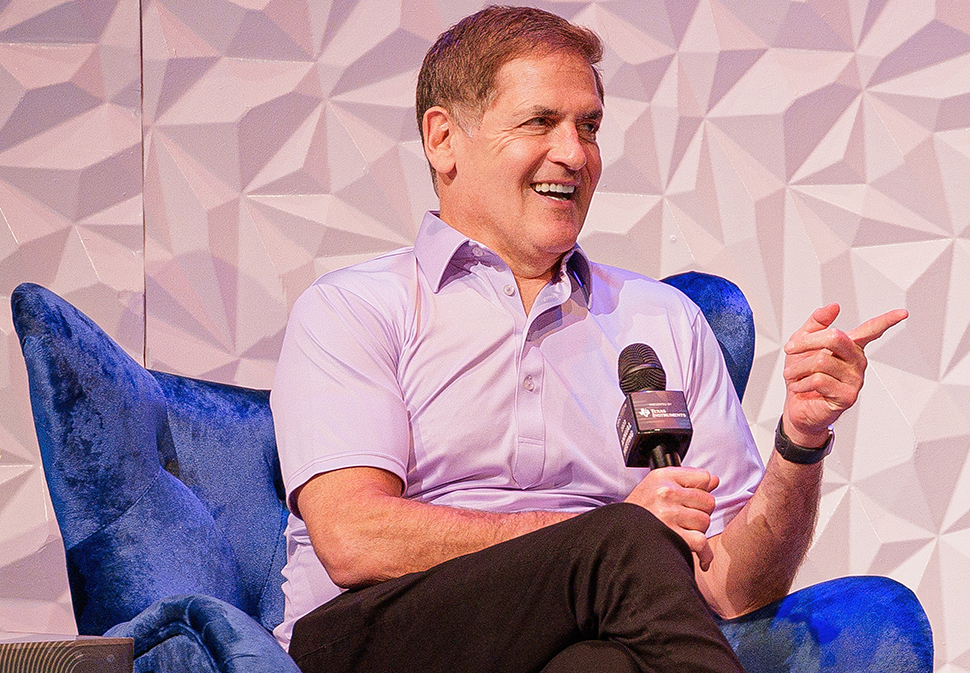
David Thompson, chairman and CEO of Osteal Therapeutics, likens PJI to a cancer-like killer, comparing the five-year relative survival rate to breast cancer. “This is a very serious diagnosis,” he said last year at the BioNTX iC3 Summit in Irving.
$50 million Series D will accelerate development
With the new funding, Osteal plans to speed up the development and launch of VT-X7, its leading candidate for treating PJI.
In June, Osteal announced it had secured an oversubscribed $50 million Series D funding round, following a $20 million Series C raise last fall. Thompson described this latest funding as an “inflection point” in the company’s mission to bring its innovative treatment for PJI, VT-X7, to market. Osteal plans to seek FDA approval for the treatment later this year after completing a Phase III trial.
With no currently approved therapies for PJI in the United States, Osteal sees a “first-mover advantage,” Thompson said.
The potential market for treatment of the stubborn infection is significant, he noted: about 45,000 patients annually, representing a $3 billion opportunity growing at 6% per year.
Battling biofilms in joint replacement complications
According to Thompson, PJI is a devastating condition whose outcomes haven’t improved in a meaningful way in over two decades.
And while admittedly rare, the risk of the joint infection is relatable: ” I could ask everyone to raise their hands on this because I already know the answer,” Thompson said onstage at iC3 last fall. “Every single person in this room either has a joint replacement or knows someone with a joint replacement.”
While joint replacements are generally successful, about 2% become infected, according to the CEO. For those people, the current treatment is a two-stage, 16-week therapy “that’s ineffective in half the patients.” And “if you’re over 65 and you get one of these, there’s a good chance you’ll never be fully ambulatory again,” he said.
Biofilm infections are complex structures where bacteria hide within a “protective polysaccharide matrix.” This matrix shields them from the immune system and systemic antibiotics, making them difficult to treat, much like cancer, Thompson explained. “You need an antibiotic to reach it to treat it,” he said.
“The biofilms grow on metal. They grow on the plastic polyethylene inserted, they grow in the bone, and they grow in the tissue,” he added. “These bugs love to make biofilms on foreign bodies.”
A need for better treatments for PJI
At iC3, Thompson said the great challenge in the market today is “that the current standard of care is long, is painful, and it doesn’t work,” he said.
Today’s standard for treatment of PJI involves a two-stage exchange arthroplasty and has a success rate under 50% after 12 months, according to the CEO. In the first stage of this traditional process, the infected joint is surgically removed and replaced with an antibiotic spacer. This spacer is not a fully functional joint, making it difficult for patients to move and live their daily lives, Thompson noted.
Following the initial surgery, patients typically have six weeks of intravenous antibiotics. This period is not only uncomfortable but also carries the risk of serious side effects, including kidney damage, he noted. If the infection clears, patients then undergo a second surgery around week 16 to implant a new joint.
Unfortunately, for about half of the patients, the infection returns or never fully clears, leaving them without a new joint, Thompson said.
Osteal’s solution? A seven-day treatment that, in clinical trials, has shown promising results. “In our phase two trial, 100% of patients were reimplanted in seven days,” Thompson said in the onstage presentation. “We take a 16-week therapy that’s ineffective in half the patients, and we make it effective in 100% of patients.”
The company’s VT-X7 approach, using a drug/device combination product for seven days, delivers high concentrations of antibiotics directly to an infection site, aims to avoid the systemic toxicity of traditional treatments, according to Osteal.
And unlike the traditional two-stage exchange arthroplasty, which can require two major surgeries (removal of the infected joint and later re-implantation of a new joint), Osteal’s treatment platform could reduce the need for multiple operations.
“Every 60 minutes of incremental operative time has been shown to increase complications by 25%,” Thompson noted. “By reducing the operative time, we not only enhance patient safety but also improve overall outcomes.”
Streamlining adoption and regulatory exclusivity
Thompson has noted the new PJI treatment platform is well-positioned for smoother integration into the healthcare system. Beyond its clinical effectiveness, it helps ensure the treatment is financially viable for healthcare providers and accessible to patients.
The CEO of iC3 noted the important benefits of coding and getting paid for VT-X7, saying that it can be billed under existing codes for treating periprosthetic joint infections, which makes it easier for hospitals and surgeons to get paid. “We have existing coding coverage and payment. So the surgeons and hospitals bill the same code they bill today,” Thompson explained.
The QIDP and Orphan Drug designations offer up to 12 years of market exclusivity, protecting VT-X7 from generic competition, he said. “The benefit of orphan drug and QIDP, that’s Qualified Infectious Disease Product designation, is really combined sequential 12 years of regulatory exclusivity on these drugs,” he said.
Thompson expects VT-X7 to qualify for Medicare’s New Technology Add-On Payment (NTAP), ensuring additional reimbursement from day one of its launch. And with 50% of potential patients treated at just 300 hospitals and 65% covered by Medicare, VT-X7’s target market is concentrated, he remarked—adding that “one payer represents a very large number of our patients.”
And, he said, the therapy’s clinical efficacy and safety make it a strong candidate for value-based reimbursement models in healthcare, which emphasize paying for treatments that deliver the best outcomes.
Anticipating a ‘roughly three-fold increase’ in annual procedures
Osteal board member and investor Martin Sands affirmed the medical need for better treatment options in the company’s Series C announcement last fall. “PJIs, while rare, closely track the number of primary and revision joint replacements,” he said at the time. “An aging population that’s seeking to stay active will drive a roughly three-fold increase in annual procedures between now and 2040.”
On LinkedIn, Sands called Osteal’s recent Series D funding a “tremendous endorsement of [its] drug device patented platform therapy.”
Zimmer Biomet representative to join the board
Medtech giant Zimmer Biomet led the Series D funding and an as-yet undisclosed representative of that company will join Osteal’s board of directors. The round was joined by returning investors Johnson & Johnson Innovation-JJDC, Inc., Gideon Strategic Partners, and HM Capital.
The company aims to leverage its investor partnerships to bolster its strategic and operational capabilities.
The privately held, clinical-stage biopharmaceutical company’s pipeline includes the development of four products in the orthopedic drug delivery devices arena, and Thompson has noted the importance of its funding partners in the development of new treatments.
“From the beginning, Osteal has been extremely fortunate to have the support of a world-class group of financial and strategic partners who share our vision and recognize the tremendous impact our programs will have on patient care,” Thompson said in a statement.
Moving from California to Dallas: “That was fantastic for us.”
At iC3, Thompson said his company’s move from North San Diego County to Dallas in 2020 has been pivotal to its progress. “That was fantastic for us,” he said. “We found the North Texas talent pool has just been outstanding. We couldn’t feel better about it.”
The CEO specifically cited the “friendly business environment and growing life science community fostered by BioNTX in North Texas” as a key factor in his company’s success.
BioNTX CEO Kathleen Otto, who leads the bioscience and healthcare innovation trade group in North Texas, is proud Osteal Therapeutics calls North Texas home. She told Dallas Innovates that the company’s success reflects the region’s strong resources in both talent and support for healthcare innovation companies.
BioNTX hosts the annual iC3 summit showcasing biotech advances in North Texas. Osteal, a 2023 BioNTX “Rising Star” award recipient, presented its “first-in-market” product candidate, VT-X7, at the group’s iC3 Life Science & Healthcare Innovation Summit, Otto said.
Commenting on Osteal’s recent funding success, Otto said that after the FDA granted Breakthrough Therapy Designation to VT-X7 last December, the company’s new funds would help accelerate the launch of its new treatment for PJI.
Aiming for FDA approval
With the recent $50 million Series D funding secured, Osteal Therapeutics plans to submit a New Drug Application upon completion of its APEX-2 study, expected in late 2024.
The FDA has previously recognized VT-X7’s potential, and its latest designation builds on Osteal’s earlier Orphan Drug, Fast Track, and Qualified Infectious Disease Product designations, the company noted. The acknowledgments could streamline the approval process, potentially bringing this innovative treatment to patients sooner.
“We expect to be approved in 2025,” Thompson said at the iC3 Summit last year.
“We are strongly poised at this point to become the standard of care within PJI,” he said. “We have very strong data showing both clinical and quality of life benefits.”
Lance Murray contributed to this report.
![]()
Get on the list.
Dallas Innovates, every day.
Sign up to keep your eye on what’s new and next in Dallas-Fort Worth, every day.