Researchers at UT Southwestern Medical Center have identified a protein that causes human cell membranes to burst during necroptosis—a form of programmed cell death.
The discovery could lead to new treatments for severe infections, inflammatory diseases, neurodegeneration, and cancer—including conditions such as Crohn’s disease, Alzheimer’s, ALS, and several tumor types.
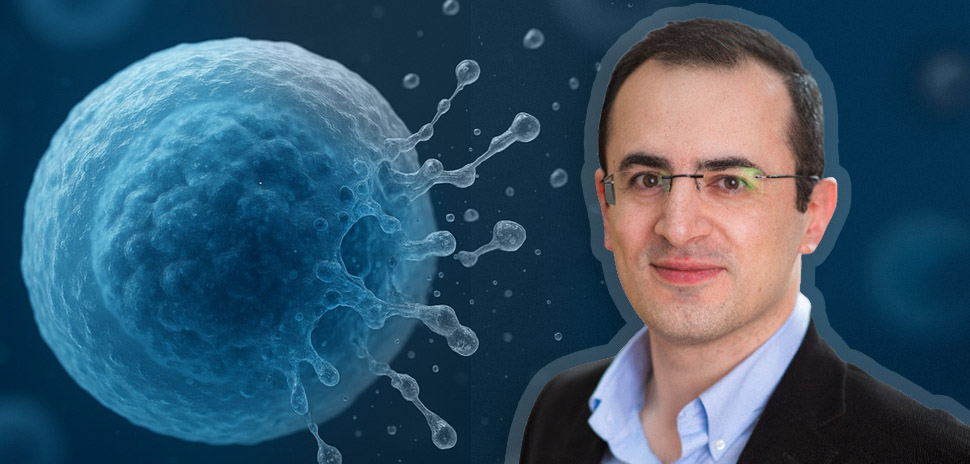
Research findings, published in Nature, identify what study leader Ayaz Najafov describes as “a previously unknown, druggable control point in inflammatory cell death.”
Najafov, an assistant professor of internal medicine at UT Southwestern, said the protein—known as SIGLEC12—acts as “a human-specific mediator of necroptotic membrane rupture.”
Why it matters
Programmed cell death helps the body clear out old, damaged, or infected cells, according to Najafov, who also works in the Cellular Networks in Cancer Research Program within the Harold C. Simmons Comprehensive Cancer Center.
But necroptosis—a specific subtype—can become harmful when inflammation triggered by infection or chronic disease pushes the process into overdrive.
As Najafov explained in a UT Southwestern announcement, necroptosis ends with cell membranes rupturing, releasing distress signals that draw immune cells to clear debris and fight microbes.
Scientists had already identified proteins that rupture membranes in other cell-death pathways—apoptosis, pyroptosis, and ferroptosis—pointing to a protein called NINJ1, he noted. But NINJ1 doesn’t appear to play a role in necroptosis, leaving a missing link in understanding how this specific process ends.
“Although previous studies have identified the preceding steps in the necroptosis molecular cascade,” the UTSW announcement said, “none had discovered a protein analogous to NINJ1 in this process.”
How UTSW researchers found it
Najafov’s team used CRISPR gene editing to knock out individual genes in human cells engineered to activate MLKL, which is the last known protein in the necroptosis cascade. Most cells underwent necroptosis and ruptured, except those in which CRISPR had disabled the gene that codes for SIGLEC12, a protein with parts “strikingly similar to NINJ1.”
When researchers pushed SIGLEC12-deficient cells to undergo necroptosis, their membranes ballooned but didn’t break. Producing extra SIGLEC12 didn’t trigger rupture either.
The team discovered that a protein, TMPRSS4, cleaves a portion of SIGLEC12, which appears to be the key activation step. Experiments using only the “cleaved” form of SIGLEC12 showed it was enough to cause membranes to burst, UTSW said.
A cancer connection
Cells from many cancer types are less likely than healthy cells to undergo necroptosis, a trait thought to help them survive and grow, the researchers noted.
Najafov and his colleagues found that many cancers carry SIGLEC12 mutations that prevent TMPRSS4 from cleaving the protein, blocking its function. They also identified similar mutations in the general population. According to Najafov, they could influence a person’s vulnerability to infections or inflammatory disease.
What’s next
Drugs targeting SIGLEC12 or TMPRSS4 could eventually be used to prevent necroptosis and treat conditions where it plays a central role, Najafov said.
First author Hyunjin Noh, a postdoctoral researcher, and graduate student researcher Zeena Hashem also contributed to the study. The work was funded by the National Institute of General Medical Sciences and a National Cancer Institute Cancer Center Support Grant.
Don’t miss what’s next. Subscribe to Dallas Innovates.
Track Dallas-Fort Worth’s business and innovation landscape with our curated news in your inbox Tuesday-Thursday.